How AI and FHIR Interoperability Are Transforming Care Coordination in 2025
In 2025, healthcare is entering a new era where AI and FHIR interoperability converge to transform care coordination across hospitals, clinics, and health networks. This blog explores how artificial intelligence automates data integration, converts unstructured clinical notes into standardized FHIR resources, and powers smarter, real-time care collaboration through Health Information Exchanges (HIEs).
10/31/20252 min temps de lecture


Every clinician, nurse, and data analyst knows this truth: Health data isn’t scarce — it’s everywhere. The real challenge is getting the right data, to the right person, at the right time, without breaking privacy rules or clinical workflows.
In 2025, AI-driven interoperability powered by FHIR (Fast Healthcare Interoperability Resources) is beginning to solve this problem — one data exchange at a time.
The Vision: From Siloed Systems to a Learning Health Ecosystem
Imagine Maria, a patient living with congestive heart failure.
She sees multiple providers — her primary physician, a cardiologist, a home health nurse, and a telehealth dietitian. Each uses different systems. Each records data differently.
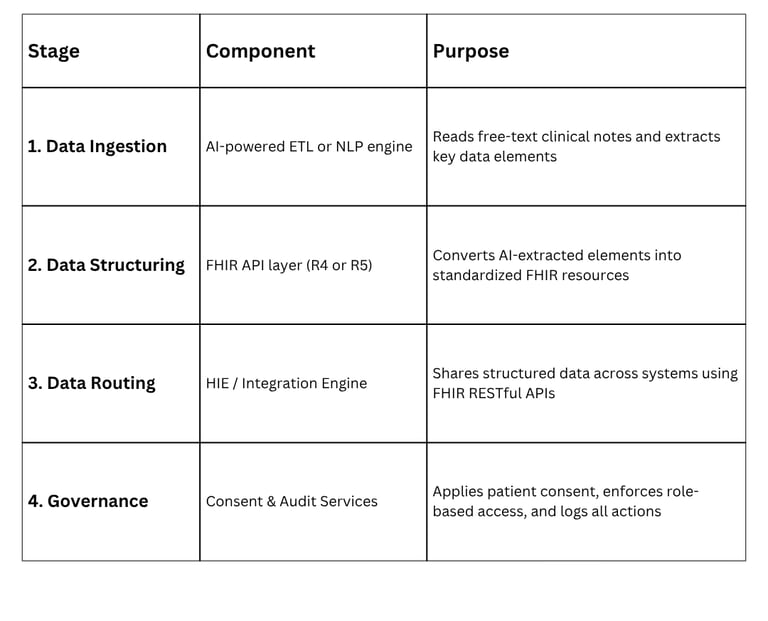
Here’s where AI + FHIR interoperability step in:
AI reads Maria’s unstructured notes — discharge summaries, progress reports, and nursing assessments.
Natural Language Processing (NLP) extracts key information like diagnosis, medication, and vital trends.
The system transforms these insights into FHIR resources — such as:
Condition → Congestive heart failure (SNOMED: 42343007)
MedicationStatement → Metoprolol 50 mg daily
CarePlan → Heart failure management, follow-up frequency, lifestyle goals
These structured FHIR resources are securely shared through the HIE (Health Information Exchange) — reaching Maria’s care team in real time.
Now, everyone sees the same information, understands the same goals, and can coordinate care without duplicate tests or missed follow-ups.
Result: Maria’s care data flows safely, accurately, and meaningfully — across every point of care.
The Role of AI in Modern Interoperability
AI isn’t just automating; it’s contextualizing.
Here’s how:
Entity Recognition: Identifies key medical concepts from free text (diagnoses, meds, procedures).
Context Awareness: Distinguishes between active vs. historical conditions.
Predictive Routing: Prioritizes alerts to relevant care team members based on context (e.g., abnormal labs to cardiologist).
Quality Assurance: Flags missing fields or mapping inconsistencies before data exchange occurs.
This blend of machine intelligence and standardized exchange means interoperability is no longer reactive — it’s proactive and intelligent.
Governance and Trust: The Non-Negotiables
With power comes responsibility. AI-driven interoperability must uphold the three pillars of digital trust:
Compliance — Systems must align with HIPAA, 21st Century Cures Act, and TEFCA frameworks.
Transparency — Patients must know when and how AI is processing their data.
Accountability — Every access, transformation, and transmission must be traceable through FHIR AuditEvent and consent directives.
Without this foundation, even the smartest system erodes patient and provider trust.
As interoperability professionals, we’re no longer just connecting systems — we’re designing ecosystems that learn, adapt, and protect.
By integrating AI-driven insights with FHIR-based data exchange, Health IT teams can:
Reduce administrative burden
Improve chronic disease management outcomes
Enable true “continuity of care” across settings
Lay the groundwork for population health intelligence
Try This AI Prompt
If you’re experimenting with AI tools like ChatGPT or your own LLM, try this prompt to explore how interoperability meets intelligence:
“As an Interoperability Lead, design a care coordination pipeline using AI and FHIR. Explain how clinical notes are transformed into FHIR resources (Condition, MedicationStatement, CarePlan), routed through an HIE, and governed for privacy and compliance. Include a visual summary of the data flow.”
This single prompt will stretch your thinking beyond data exchange — into the future of intelligent, compliant, and patient-centered interoperability.
Health data is only as powerful as the story it tells — and the systems that let it speak.
As Health IT professionals, our goal isn’t just integration.
